Guidance in preparing for the worst
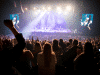
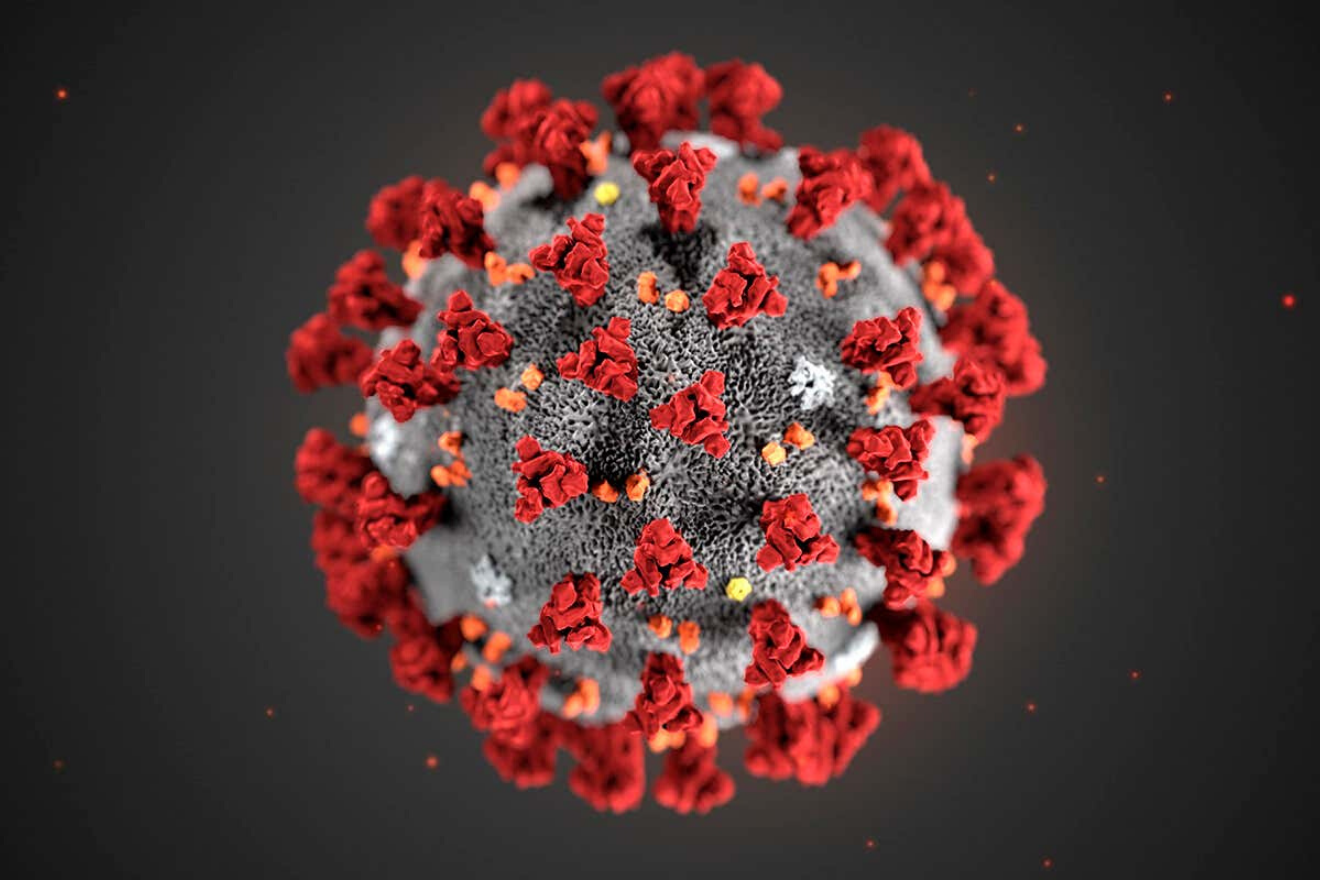
Last Friday, the World Health Organization (WHO) released a comprehensive nine-page document with key recommendations for those planning large events — “mass gatherings” in WHO’s lexicon — in the context of the COVID-19 coronavirus outbreak. Planners are likely to be familiar with many of the document’s recommendations — to be in contact with both local and national public health authorities, for example, and to communicate preventative measures to attendees, including respiratory etiquette and hand hygiene.
But other recommendations expand on standard advice for making risk assessments, including the recommendations that event planners consider the crowd density; the nature of contact between participants, including the layout of meeting venues; whether participants are registered or non-registered, and therefore easy to locate after the event concludes if necessary for public health reasons; their profession and related possible exposure risk; the number of participants coming from COVID-19–affected countries within the previous two weeks; and the average age of participants, since elderly groups appear to be more affected.
The following are basic general principles for reducing the transmission of the COVID-19 virus, excerpted from the WHO document:
- Participants and staff should stay away from events when ill
- Promote hand hygiene and respiratory etiquette, including with informational materials that reach a wide range of age groups and varying reading and educational levels
- Soap and water or alcohol hand-sanitizers and tissues should be easily accessible in all common areas, and especially in areas set aside for medical treatment
- Reduce crowding
- Isolate persons who become ill
- Where possible, event organizers should consider distancing measures to reduce close contact among people during a large event (e.g., increasing the frequency of transport and staggering arrivals and minimizing the number of people who congregate at one time at sanitary stations and food and water distribution areas)
- Organizers should plan for the likelihood of persons becoming ill with fever and other symptoms of COVID-19
- Establishing isolation areas in on-site medical treatment clinics/facilities where such persons can be initially assessed and triaged should be considered. Persons who are ill can be provided with a mask to help contain respiratory droplets generated from coughing and sneezing. The isolation area should be equipped with the necessary supplies to facilitate hand hygiene and respiratory etiquette. In addition, medical staff attending persons who are ill should wear a mask, then dispose of it immediately after contact and cleanse hands thoroughly afterwards
- In case of symptoms suggestive of acute respiratory illness before, during, or after travel, travelers are encouraged to seek medical attention and share travel history with their health care provider.